Health Plan Solutions
Maximize Quality of Care
To effectively improve the patient experience, Medicare Advantage STAR Ratings, and Quality Bonus Payment opportunities, health plans must first be able to accurately measure and assess the member experience. Seamless member interactions accelerate improvement of quality of care, increase retention, understand disenrollment, and increase market share.
Foster Collaboration Between Health Plans and Provider Networks:
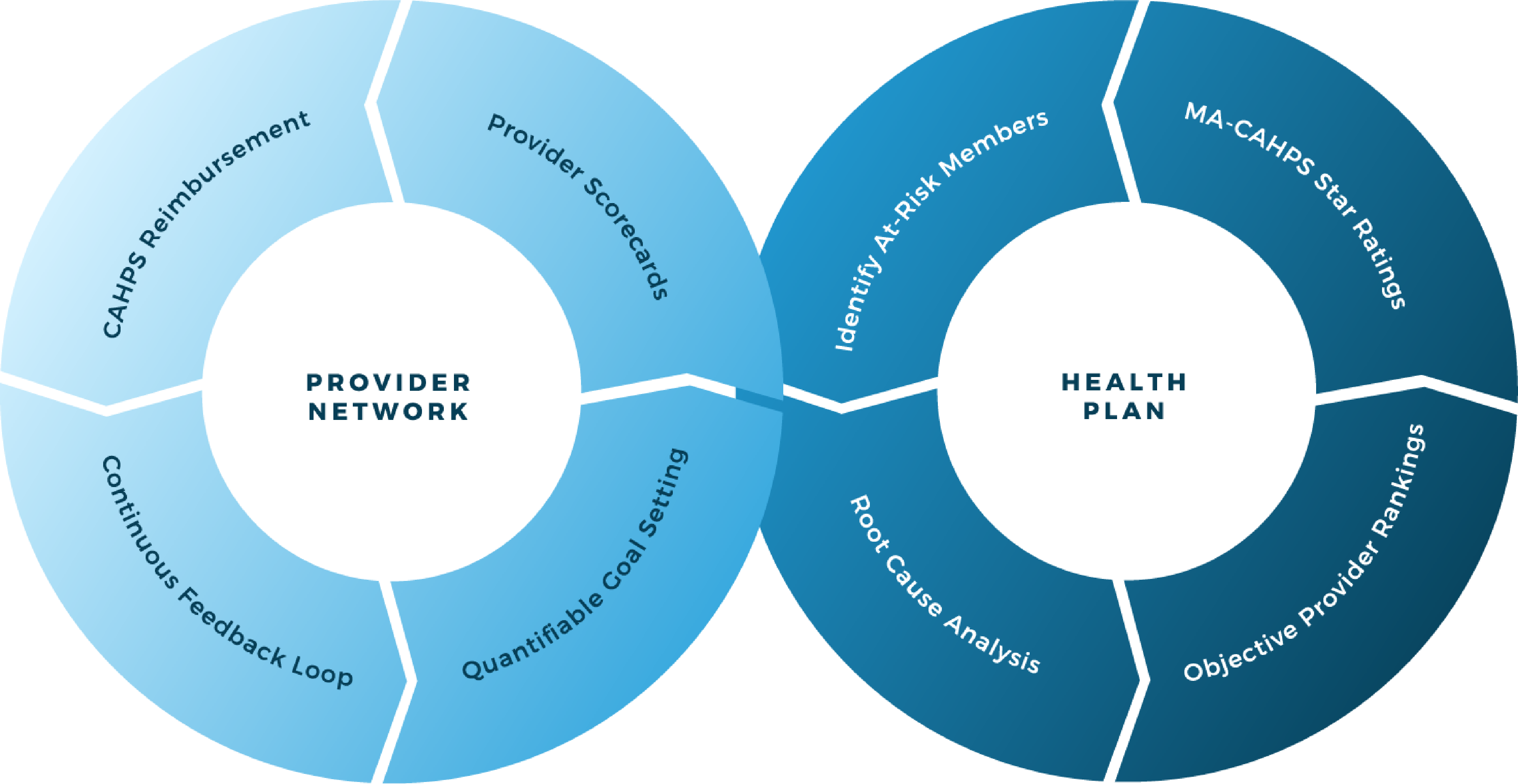
Provider Network Enagement
Provider Network Engagement surveys allow medicare advantage health plans to directly involve and potentially incent their provider networks to impact the quality of care members receive.
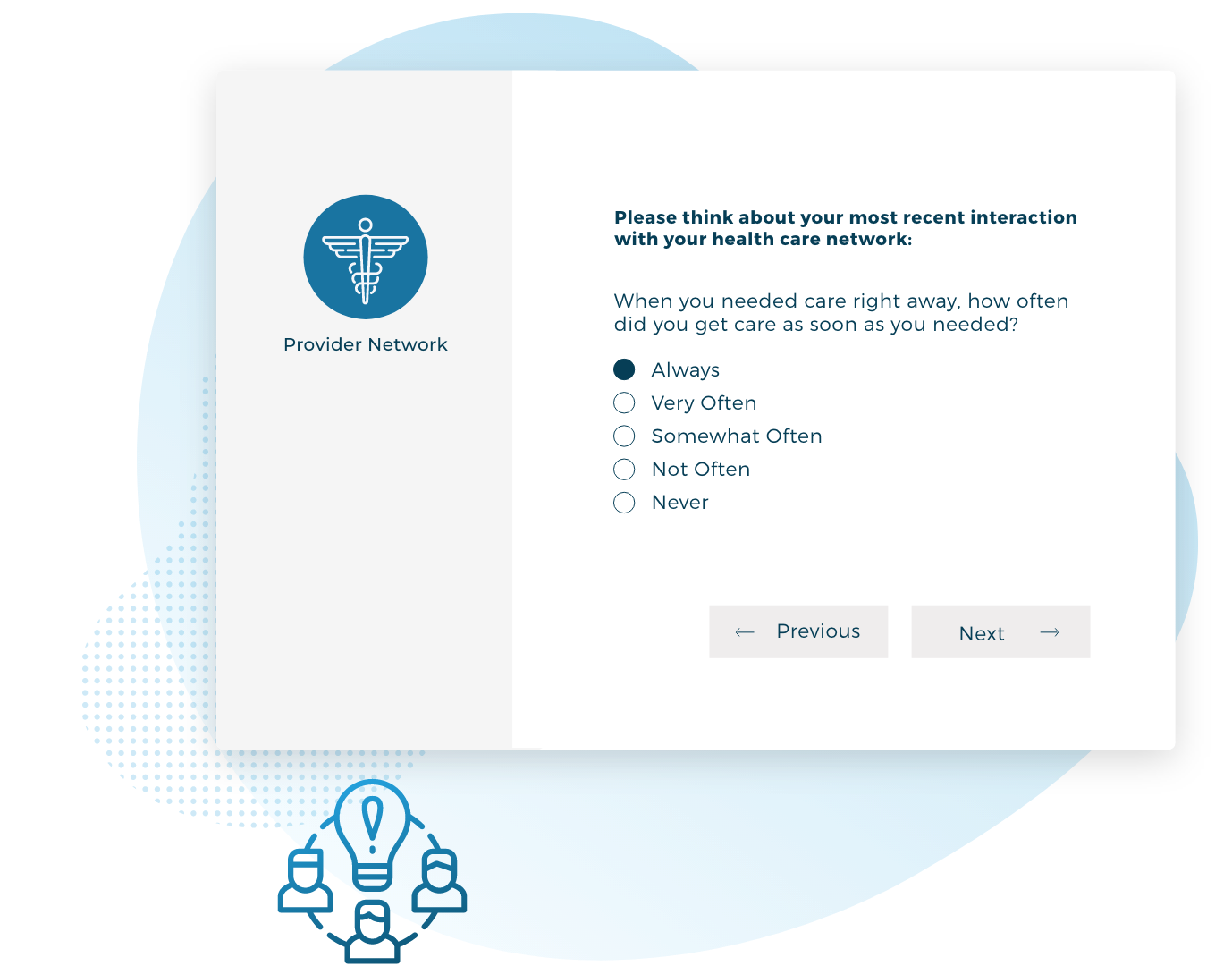

Provider Perspective
The provider perspectives survey is designed to uncover important nuances that can negatively affect a member’s experience and satisfaction with their care. Routine provider engagement surveying is an integral component in leading health care delivery in the community and becoming the health plan of choice for patients and physicians.
What We Do
Take a live tour through our Patient Experience Analytics Portal to see in detail what we can offer.
