In December 2022, we gave our recommendations on how to improve Star ratings by improving member experience. This topic is worth expanding on as a strong relationship between carrier and provider can significantly improve Star ratings. So, let’s dive deeper to determine how carriers can work with providers to improve member experience. But first, a quick refresh on why member experience matters.
Member Experience and CAHPS Surveys
Although member experience has always been a component captured by CAHPS surveys, in 2023, it is even more critical. 2023 MA CAHPS surveys will measure member experience at four times the weight it has been in previous years. As such, achieving a 4 or 5 Stars rating will only be possible with particular attention to a positive member experience. Furthermore, what happens between providers and members is a crucial component of Star ratings. Carriers should identify gaps in quality of care and communicate these with providers in order to determine what needs to be fixed and how to improve it. Maintaining the status quo on a carrier’s Star rating is insufficient, as the threshold performance will likely increase in 2023.
When carriers engage with provider networks, quality of care will be improved, and financial benefits will follow suit. Member experience should be a top priority for both carriers and providers due to its impact on revenue. Better member experience can lead to reduced operational costs for carriers. Members will be less likely to be dissatisfied with their network’s providers or use customer service tools, for example.
Member retention also impacts the bottom line. When a member is new to a plan, this is a perfect time for both carriers and providers to ensure they have all their questions answered. Once members are sure they are welcome and heard, they will likely stick to their carrier.
Improving member experience will also help carriers retain their own employees. Organizations that invest in customer experience tend to report higher employee satisfaction.
What Carriers Can Do
People-First Approach
Carriers and providers should adopt a holistic perspective on member experience. But what does this look like? Let’s say a health incident prompts a member to engage with a provider. For example, a member becomes ill or injured. First, a member must determine which providers are in-network. They can do so through a (hopefully) seamless interaction with the carrier website. Once they have selected a doctor, they make an appointment. The appointment should be within a reasonable time frame. When the member arrives at their provider’s office, they should be seen in a timely manner.
Every step along this member’s journey will lead to either a positive or negative experience. Members who can get an appointment with an in-network provider within a timely manner and receive a course of treatment will result in better survey results and Star ratings.
Within Medicare Advantage (MA) specifically, carriers and providers must adjust accordingly as seniors have certain requirements. MA members are a large population segment as MA plans have risen steadily since 2014 and will reach nearly 34 million people this year. Carriers can educate providers on what other services are available to these members, such as telehealth, if traveling to a provider’s office presents a challenge.
One area of concern carriers can communicate to providers is the mental health affecting the physical health of seniors. Providers should aim to treat members holistically, as there may be more to the picture than physical ailments. Depending on the plan, carriers can let providers know if access to mental health services is offered and in what capacity. MA members especially should feel that they are listened to and that their concerns are valid. Unfortunately, many of these members live in isolation, so exuding compassion around this reality is essential to quality care.
As quality of care improves for members, so will financial compensation for carriers. For example, MA plans with high Star ratings (4 or more) earn a bonus on CMS payments and higher rebates. Creating a positive member experience benefits them, their providers, and their carriers.
Build Trust with Providers
A vital component of a fluid health care journey is alignment between carriers and providers. To this end, carriers should work to build trust with providers. This can be a strained relationship, but it doesn’t have to be. Let’s start at the beginning: the point of contact between providers and carriers. One suggestion is to designate a particular provider as the point of contact instead of a contract manager. Carriers should do their best to communicate with providers the array of benefits available to members.
Carriers need to retain providers to keep associated costs down. In-network providers are essential because they meet the quality standards of the carrier and accept a specific rate for their service since they’ll be seeing a high volume of patients by being part of the carrier’s network. In addition, it is beneficial for the carrier to encourage providers to seek longevity.
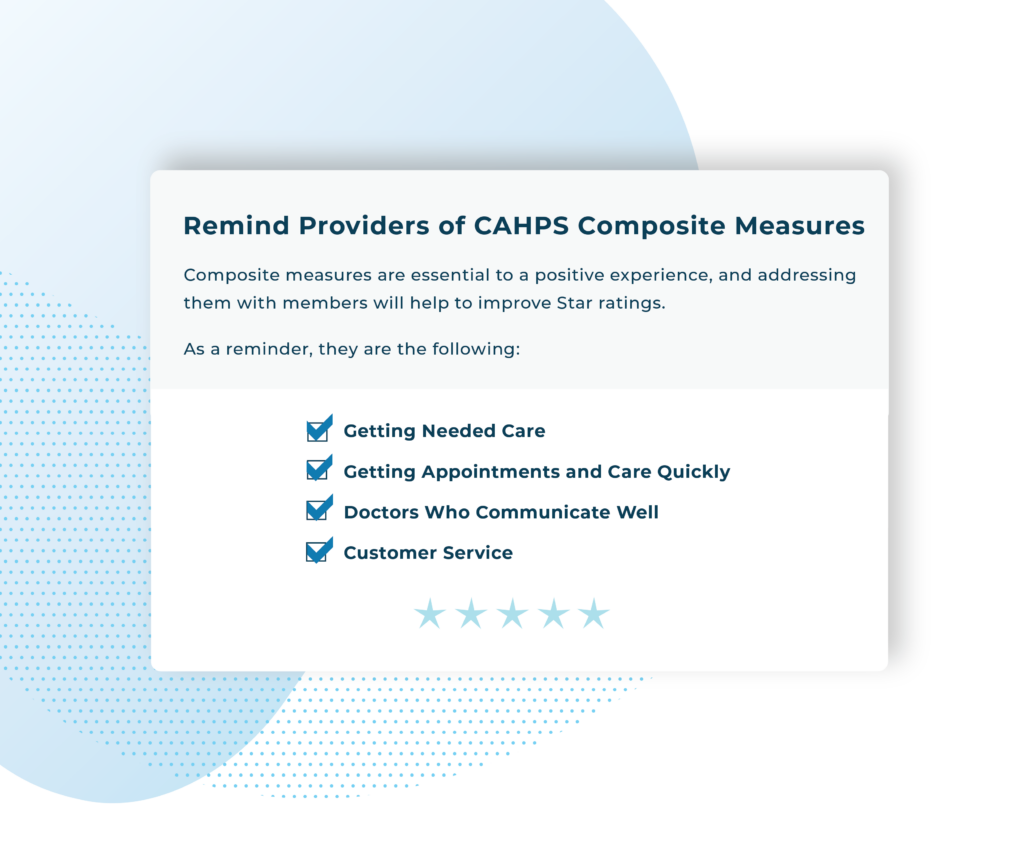
Remind Providers of CAHPS Composite Measures
Carriers should remind providers of the six composite measures included in CAHPS surveys. These should be top of mind for them when interacting with members. Composite measures are essential to a positive experience, and addressing them with members will help to improve Star ratings.
Six CAHPS Composite Measures:
- Getting Needed Care
- Getting Appointments and Care Quickly
- Doctors Who Communicate Well
- Customer Service
- Getting Needed Prescription Drugs
- Care Coordination
Recommend Continuous Surveying to Providers
Continuous surveying can help improve CAHPS scores and Stars ratings. Since member experience represents 57 percent of overall Stars ratings in 2023, carriers should regularly capture members’ concerns. Once a carrier has this data, it can empower them to take action by targeting negative scores and addressing issues promptly. Continuous surveying will ensure that a carrier and provider have fewer surprises when CAHPS surveys occur.
Want to find out how Brenmor surveys can improve your CAHPS scores? Speak with an expert today.