MIPS and Data Collection
At the midpoint in the MIPS timeline, many clinicians are focused on performance categories and payment impacts. With some of the changes in the 2022 performance year, it is important to consider some of the ways that data collection and analysis can impact MIPS scores.
The 2022 performance year brought some changes to the MIPS scoring structures, including some shifts in the weights of the quality and cost categories (quality decreased from 40 percent to 30 percent and cost increased from 20 percent to 30 percent) as well as an increase to the threshold for avoiding negative payment adjustments (up from 60 percent to 75 percent in 2022). Those not participating this year will receive a 9 percent penalty on their 2024 Medicare Part B payments. Another thing to note for the 2022 performance year is that it is the last year for additional adjustments for exceptional performance. The threshold for exceptional performance is 89 points.
MIPS Improvement Activities
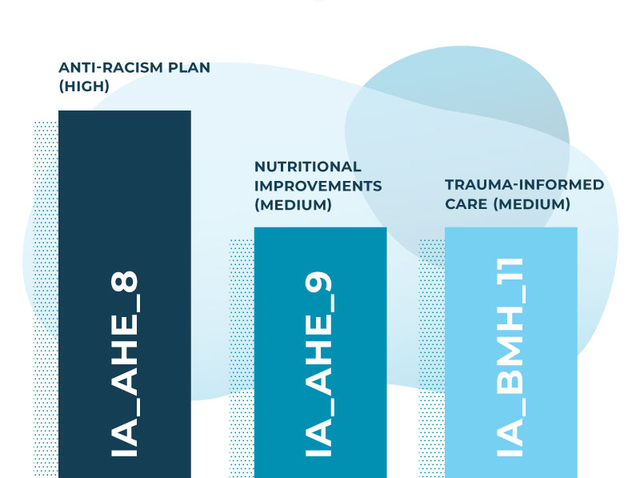
The 2022 performance year also brings some changes within the scoring categories. In relation to data gathering and application, the Improvement Activities performance category is noteworthy. This category is worth 15 percent of the overall score with a maximum point value of 40. High-weighted activities receive 20 points, and medium-weighted activities receive 10 points, giving clinicians flexible options for choosing activities. Patient experience is a key factor in the Improvement Activities category, through a number of existing activities and changes made in the 2022 performance year.
Many of the changes in the 2022 performance year reflect concerns for health equity with the addition of 7 new Improvement Activities, 3 of which are related to promoting health equity and the modification of 15 current Improvement Activities, 11 of which address health equity. With focus on equity, understanding how patients are accessing care and what barriers might be in place is an important consideration in terms of the scoring in this category.
New Health Equity Improvement Activities
Creating a Roadmap
The expansive Improvement Activity inventory offers a lot of options for making targeted and meaningful decisions about where to focus your time and resources, but one common factor to consider is data validation. Understanding where your data sources are and how to make the best use of them is key.
For a number of Improvement Activities, patient surveys can be an agile source of information and documentation, especially in areas related to health equity. Surveys can help identify gaps in access to or satisfaction with care (e.g. analysis of demographic data and satisfaction ratings) and they can be used to identify possible interventions (e.g. analysis of patient feedback). When surveys are integrated with Electronic Health Records, data gathering can be a continuous and targeted process.
Data Analysis at Work
While data gathering is an essential step in the process, equally important is what to do with that data once it has been collected. That is where survey providers come in. Having a partner that offers comprehensive solutions for outreach as well as robust data reports and analytics can make processes like MIPS reporting much less daunting.
With the ability to pair demographic information with patient feedback, surveys provide data sets that can address complex questions about who patients are, what factors might impact their access to care, and how clinicians can address issues. Data can be organized by question and sorted by identifiers to determine where interventions might be needed. Here at Brenmor, we recently worked with a client on one of the Improvement Activities using analytics tools that allowed them to see demographic breakdowns as they related to specific survey questions.
Case Study: Addressing Activity Improvement IA_EPA_3: Collection and Use of Patient Experience and Satisfaction Data on Access
This particular Improvement Activity is explicitly tied to patient satisfaction as it relates to access of care, and it includes patient surveys as one of the options for validation documentation.
Description: Collection of patient experience and satisfaction data on access to care and development of an improvement plan, such as outlining steps for improving communications with patients to help understanding of urgent access needs.
Validation Documentation: Evidence of documented improvement plan for access to care and quality based on collected and stratified patient experience and satisfaction data. The goals for improvement can be defined broadly or within certain population strata. CMS examples of stratification may include patient demographics such as race/ethnicity, disability status, sexual orientation, sex, gender identity, or geography. (It is acknowledged that some stratification data may not be available). Include both of the following elements:
1) Patient experience and satisfaction data on access to care – Data collected through a patient experience survey for a population defined by the eligible clinician. For example, eligible clinicians could give the survey to all patients seen within a defined study period. Data can be prepared in any useful format, or as they were collected; AND
2) Improvement plan – Documentation of an improvement plan, which should include specific activities, goals, and outcomes for addressing access to care. For example, an eligible clinician may observe that non-English-speaking patients were not confident in their interactions with eligible clinicians because of language barriers. A possible plan could include using translators, remote translation services, or language training. The improvement plan would include details regarding who would be trained with timelines for completion.
For this project, we looked at responses for two survey questions related to access.
- When you contact the office, how would you rate getting the help or advice that you need?
- When you contact this provider’s office to get an appointment, how would you rate getting an appointment as soon as you needed?
To help the client address the Improvement Activity, we sorted the data for each question according to two demographic identifiers: age and gender. This allowed us to see if there were noticeable differences in patient satisfaction across these demographics. Initial findings showed more variation across age groups, so we focused there.
With the data we had, we were able to dive even deeper and look at demographic categories alongside timestamps to determine if there were intersections with particular age groups and times of year that affected patient satisfaction. In the end, the data showed that there was a particular demographic age group that scored lower, both overall and across each timeframe. The availability of the right data and the right analytics allowed the client to identify a demographic group and develop a plan to improve patient satisfaction within that group.
This project is just one example of how patient surveys can be used to identify potential issues and develop interventions for them, as well as provide solutions for CMS reporting.
Making Data Work for You
There are a few approaches to working with data that depend on where you are in the data gathering cycle. You can start with a question and build your data sources around it, or you can examine existing data to see what kinds of stories are emerging. In either case, patient surveys can paint a detailed picture.
Whichever side of the data story you start with, it is important to make your data set as comprehensive and complete as possible. This is especially true of patient surveys. On the data gathering side, distribution should be as wide and accessible as possible to ensure a representative sample, and on the data analysis side, having access to responsive reporting and analytic tools can help you make the most of your data sets.
To learn how your organization can gather continuous, year-round survey feedback, speak with an expert today.
