Lasting Effects from COVID
It is no secret that the pandemic has had a lasting impact on health care systems, and in turn, on patient experience. As defined by AHRQ, patient experience is “the range of interactions that patients have with the health care system, including their care from health plans, and from doctors, nurses, and staff in hospitals, physician practices, and other health care facilities.” There are a variety of challenges facing health care and plan providers that bring patient experience front and center. So far, this year has found many of the major health care providers in difficult financial situations. Outpatient visits are increasing, but staffing shortages and higher operating costs have created a new challenge. For plan providers, this year comes with big changes to the Star Ratings, putting greater emphasis on patient experience than in previous years. Additionally, systems are seeing high levels of churn, making ratings more important than ever.
Provider Challenges and Opportunities
There are a number of struggles for health care providers right now. Existing issues were exacerbated and new issues have arisen. With all of the stressors, creating excellent patient experiences is more difficult, but also more important. Patients are dealing with fear and anxiety and outpatient visits have had to be deferred to accommodate surges in COVID cases. Providers are now faced with a complicated problem. How can they make sure patients have positive experiences with their care while resources are strained?
Financial Losses
Many of the major providers, including Mayo Clinic, Kaiser Permanente, and Trinity Health reported substantial losses during the first quarter of the year. This downward trend can be tied, in large part, to the pandemic. The first part of the year saw another surge in COVID cases, which for many systems resulted in cancellation or deferral of elective procedures. Coupled with major labor shortages, rising labor costs, decreased federal funding, and investment losses, this makes for a difficult balancing act.
In a time when health care providers are having to do more with less, ensuring quality care and a positive patient experience is challenging, but essential. Having an in-depth understanding of patient experience can help providers make the most of the resources they have available.
Staffing Shortages
While staffing shortages are not a new phenomenon in the healthcare industry, they have certainly intensified during the pandemic. According to a 2021 Morning Consult report, nearly 80% of the health care workers they surveyed reported that they had been affected by the labor shortage. Respondents cited things like long hours, burnout, and patient loads as contributing factors.
Through the pandemic, health care workers have faced increasingly demanding working conditions, causing many to leave their jobs. The Morning Consult survey found that nearly one in five health care workers have quit their jobs since the start of the pandemic, and of those who remained, nearly one in five has considered leaving the field.
The impact of staffing shortages is twofold. Most obvious is the direct impact on patient care from increased patient loads, additional hours, and burnout. On the other side is the financial impact from wage increases to attract candidates or to bring on contract workers, which adds to the strain on resources.
Data-Driven Decision Making
While this is a time of great difficulty for health care providers, it is also a time of opportunity. The pandemic has shed light on some long-standing issues in the health care industry, and there is an opportunity to make meaningful changes. In order to really understand where change is needed, it is imperative that health care providers have an understanding of how their patients are experiencing health care.
In an interview for the Beryl Institute’s podcast, To Care is Human, President and CEO of Virtua Health, Dennis Pullin, talks about his philosophy. “The person who thinks he knows everything…has the most to learn. And so even as a CEO, I find that I do better when I listen and I observe and I gather facts, and I try to be as informed as possible.” He describes his company’s strategy to orient to the consumer by listening to patient concerns and gathering feedback. The data they gather gives them a better understanding of overall patient experiences and trends so they can address issues.
Patient feedback can also help address issues like equity. In the interview, Pullin talks about the work his company has done to address equity, and points again to the importance of patient feedback. “Equitable care doesn’t mean the same experience for everyone. In order to address equity, you have to first recognize where people are coming from and shape the experience to match it.” Patient experience and satisfaction surveys are powerful tools in the effort to provide the best and most equitable care for patients.
Plan Providers and Impacts of Star Ratings
Member experience is playing an increasingly large role for plan providers with recent and ongoing changes to Star Ratings. Due to changes in Star Ratings over the past year, the weight of member experience in the ratings has increased by 6% and is expected to increase by another 17% with additional changes coming in 2023. With member experience accounting for such high percentages of the ratings, it is essential for plan providers to understand member needs and concerns.
Ratings Increases
The number of plans with 4- and 5-Star ratings has increased significantly more in the past year than in previous year-to-year comparisons. Plans with 5-Star ratings saw a major jump in the past year compared to the previous year. From 2020 to 2021, the number of plans with 5-Star ratings went from 20 to 21, but in the past year, that number has increased to 74. The number of plans with ratings of four or four+ Stars jumped from 110 to 152 and from 63 to 96, respectively. These increases in ratings have significant effects on members and providers.
A recent article from Healthmine outlines the impacts. “These strong ratings unlock the maximum available quality bonus payment and rebates to fund rich benefits for members. More importantly, the normally elusive 5-Star rating allows all of these plans to market their products throughout the entire year in 2022, providing them with a strong local competitive advantage.”
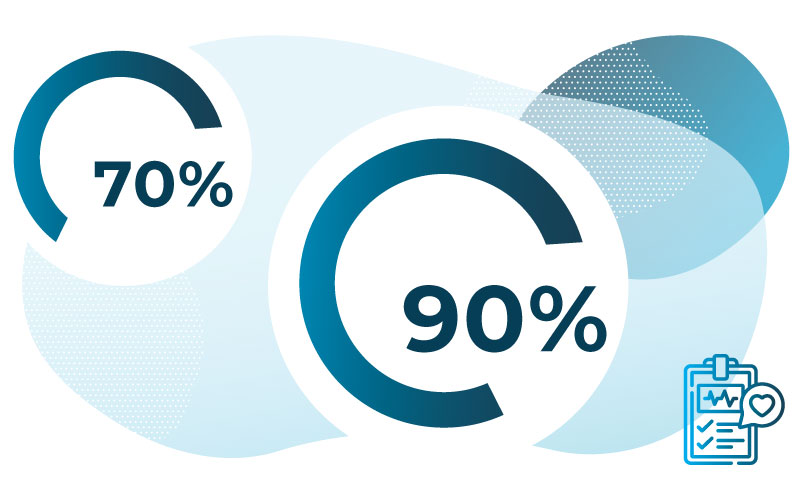
The article also reports that “almost 70% of all MA plans are now at 4 or more Stars, providing quality bonus payments to almost 90% of all eligible beneficiaries.”
It is important to consider these numbers in context. As ratings measures change and some of the COVID-related safeguards are removed, the ratings in 2023 and beyond may look different.
Impact of CAHPS on Star Ratings
The relative impact of member experience has increased with the increased weight of CAHPS on Star Ratings. The weight changed from a 1.5x to 2x in 2021, and is set to increase yet again in the coming year to 4x, making member experience a top priority.
During a recent panel discussion, Kempton Presley, Chief Analytics Officer for AdhereHealth, described the correlation between CAHPS performance and Star Ratings. Ninety-six percent of plans achieving 4 Stars or above in CAHPS also reached 4 Stars or above overall. These higher performing plans also had significantly lower member attrition rates than other plans. Sixty-five percent of plans with 4 Stars or more in CAHPS kept their attrition rate below 10 percent.”
For health plan providers, patient experience will be a driving factor in market share, bonuses, and member benefits. If providers want to see increases in CAHPS scores, they have to have a fine-grained understanding of how patients view their plans in order to deliver high-quality experiences.
Proactive Approach
The goal for health care systems is to provide the best and most equitable care for their patients, and increasing focus on patient experiences in CMS ratings are part of that overall picture. However, CAHPS is only one part of the puzzle. In order to really improve patient experiences, it is important to regularly collect feedback and work to understand the wide array of patient experiences from a fine-grained and nuanced perspective.
To learn how your organization can gather continuous, year-round survey feedback, speak with an expert today.
