Provider Network Engagement
Improve Quality of Care and Market Share
Even minor improvements to a Medicare Advantage health plan member’s experience can add tens of millions of dollars of revenue by driving higher brand preference, lower cost of acquisition, and reduced churn.
Surveys Measure CMS Regulatory Composites

Payer experience
- Supplemental benefits
- Customer service
- Overall satisfaction

Office experience
- Access
- Staff
- Wait times

Net promoter scores
- Likelihood to recommend provider
- Provider evaluation
Member Engagement and Provider Collaboration
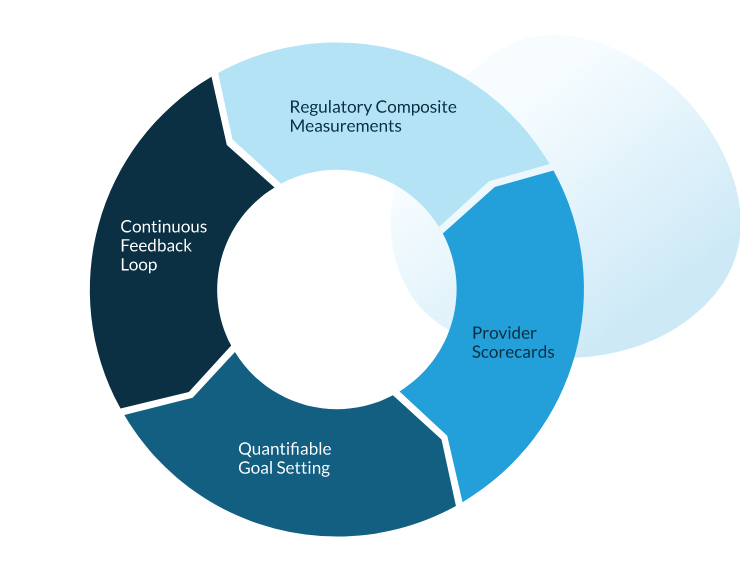
Medicare Advantage health plans can’t rely on a single, low-response survey per year for an accurate snapshot of member experience and quality of care. Our provider network engagement solutions aim to engage members to provide feedback on the quality of care at the network.

What We Do
Take a live tour through our Patient Experience Analytics Portal to see in detail what we can offer.