Medical Group Solutions
Data-driven Improvements
We empower medical groups to make patient perception a priority, as well as prepare them for public reporting so they can maximize reimbursements.
Our Patient Experience Analytics Portal provides real-time access to both current survey results as well as historical survey performance. Executive dashboards provide quick access to the most frequently used KPIs and survey information. Customizable report-builder tools allow report templates to be saved for future use and utilized to deliver scheduled reports to key decision makers.
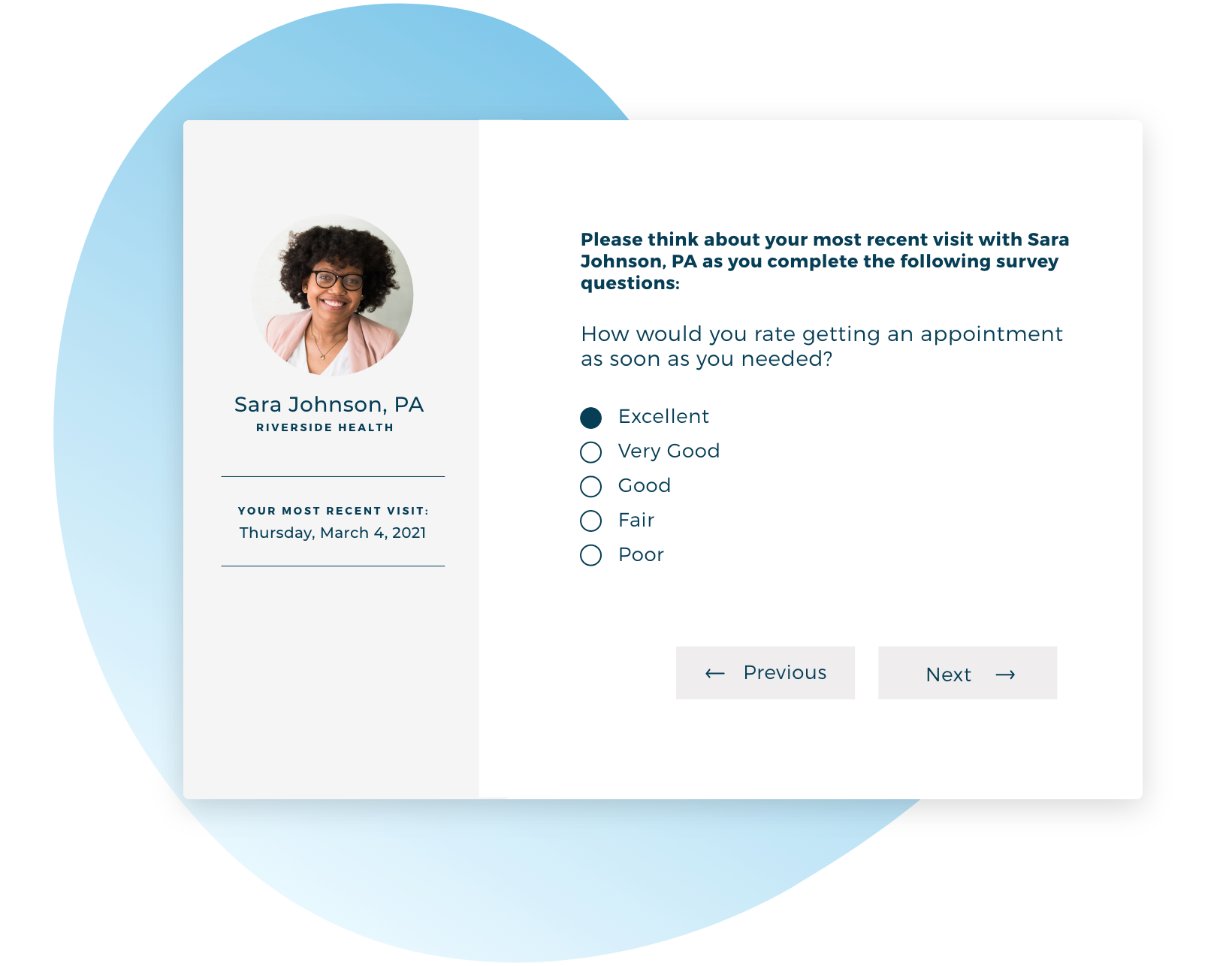
Patient Experience Surveys
Customizable surveys are designed to cover all critical practice areas and are a statistically reliable and cost-effective way for practices to identify areas of opportunity.
- Close care gaps
- Maximize reimbursements
- Organizational improvement
- Prepare for annual CAHPS reporting
- MIPS
- CG-CAHPS
- ACO CAHPS
- Robust, digestible data analytics
- Minimize survey fatigue
Provider Engagement
Proactively solicit feedback from physicians about a number of key themes:
- Clinical operations
- Leadership and management
- Technology systems
- Work-life balance and compensation
- Topics of interest


What We Do
Take a live tour through our Patient Experience Analytics Portal to see in detail what we can offer.